As a water and scientific centric community, much of our focus is centered on emerging contaminants, challenges in treatment, new technologies, or whether that beer made from recycled water can really be trusted. These topics often leave me brain-drained, wondering if I will be able to retain or understand any of the information I just received. That drain is relatively easy to overcome once I get back home, get some rest, and focus on life outside of work. There is however, a lingering drain on my psyche this time of year, leaving myself and likely others, feeling pressured to make major changes at all levels when it comes to the conservation of water. Reading about droughts, water shortages, or companies taking water improperly with little to no punishment (*ahem* Nestle!) can be mentally taxing.
I often wonder if I am doing enough to help conserve water and reduce usage in my household, while simultaneously convincing myself “there’s only so much I can do.” In fact, there is SO MUCH I can do! Lately I have found that the smallest of changes throughout my day have improved my mentality with regards to being water conscious, and I wanted to use this month’s blog to remind us of some well-known, as well as relatively unknown methods of conserving water. If I can reduce my water usage by just one gallon a day, then that means one to two days’ worth of an individual’s recommended fluid intake is available for use elsewhere, or at least not being used unnecessarily! Stringing any number of the methods below can increase that number drastically. How many measures can you add to your daily routine?
The Obvious:
You’ve likely heard of or implemented these steps already, but it wouldn’t be a list of water saving tips without them!
-Fix leaks, replace washers, limit drips: One of the best ways to reduce water use is to eliminate uncontrolled use of water. Washers are cheap, and in hoses they are simple to replace, start there if you find leaks on the way to the yard or garden. Sink faucets take a bit more time, but washers can easily be replaced (a quick google helps if you are unsure). A leak that drips just once a minute can amount to roughly a liter of water a day, but often drips occur at ten times that rate.1
-Reduce shower time: One minute off your shower time can save 2.5 gallons based on the average showerhead, according to the EPA. Any amount of time you can shave off here adds up quickly!
-Install low-flow shower heads and toilets: More efficiency and less flow means less water use, easy fix here if you can install your own. If renting like myself, you can always reach out to the landlord about making these minor changes and the importance of reducing water usage. If not for you, maybe they will think about making the switch between tenants!
-Don’t let water run in general if not in use: This goes for all tasks water related, if it’s not actively in use, make sure the faucet is off. Brushing your teeth, washing your hands, doing the dishes, all of these involve the use of the faucet, but not the entire time. One minute of faucet use can equate to a gallon of water at an average flow setting.2
The Less Obvious:
Some of these may come into play on a daily basis already, but some less apparent methods for saving could be added in!
-Collect water for general use rather than letting it flow down the drain: Nobody wants to jump in the shower right as you turn the faucet on. If you really want to go into full water savings mode, use a bucket to collect the cold water as the shower warms up, then use it on general tasks around the house: watering plants, watering pets, rinsing dishes, cleaning in general! This can work in any scenario where you may need to run water until it reaches a desired temperature. Collect water in a pitcher to put in the fridge for cold drinking water later rather than running the faucet until it is cold (I suppose ice is a thing too…)
-Drink tap water over bottled: Aside from the impact plastic has on the environment, it also takes at least twice as much water to make a plastic bottle than then bottle can hold. Reusable bottles or cups all the way!3
-Defrost food ahead of time in the fridge: Rather than setting the food in water, or running water over it to defrost.
-Use the garbage disposal less frequently: Scrape food waste off into the trash as much as possible, disposals require running water to be effective. This can also reduce the time required to rinse off dishes in general.
-Wash dishes and laundry in full loads: Math would dictate that 2 large loads of laundry uses less water than 3 medium loads. I can always count on finding random clothes or hand towels that can fill up a load if I really need to get a smaller set of clothes washed!
-Find efficiency in the garden: I could create a whole blog on garden efficiency itself! There are plenty of venues to save water here:4
- Mulch around plants to allow for less evaporation of water
- Water locally near the base of the plant
- Don’t water if the soil is still visibly wet
- Use drip irrigation if possible
- Collect water for outdoor use during rain events – Most areas in Colorado now allow for the collection of up to 110 gallons of rain water to use on the lawn or garden.5 Or use that water collected from the methods above!
- Water in ground plants in the morning to reduce evaporation
- Plant native vegetation where possible, they are used to our arid climate
- Mow the lawn higher and with sharp blades, both can reduce water use of lawns
- Install timers, forgetting a running sprinkler is great for the lawn in the short term, but terrible for water conservation all around (guilty as charged..) They can also be delayed, or sense rain events to reduce unnecessary watering
The Unknown or “Life Changers”:
These methods are further removed from water itself and may require a good deal of work to implement on your own and as a population. Producers will produce so long as customers continue to use their products, so it takes a large group of individuals making adjustments over time to see real change, but it can be done! Props to those of you who may already be participating in the following:
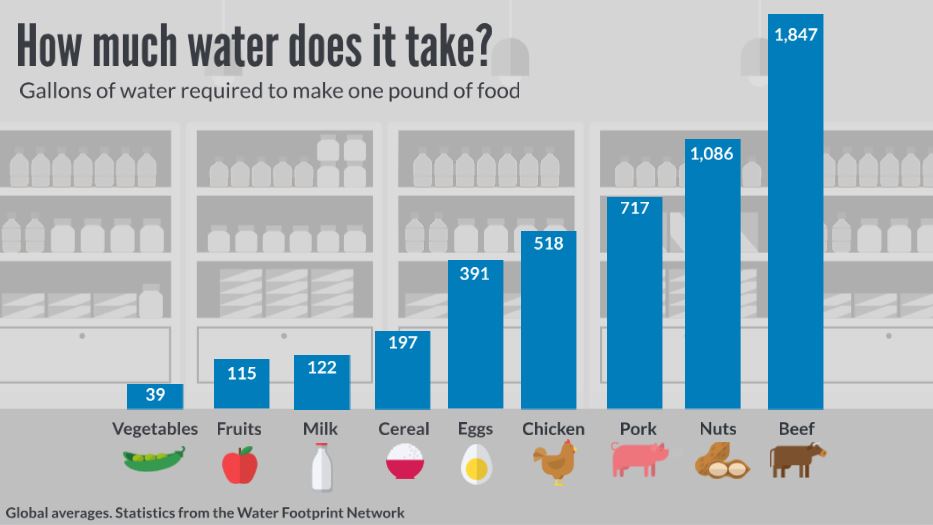
-Eat less meat: Some of you reading this have likely already taken this route, so you are well ahead of my water saving footprint! Meat products require water use in keeping the animals alive directly with water, as well as growing their food source. Fruits and veggies cut out the middle man (middle cow?) and only require a water source and some TLC. Even substituting a beef meal with a chicken meal can provide a major reduction in water usage! Denver Water helps highlight the differences in water usage among food sources in this article.
-Drive less when possible: It requires roughly 2.5 gallons of water to refine a single gallon of gas. Why not combine climate benefits with water resource benefits and walk or bike to those nearby locations instead? If nothing else, do your best to avoid hoarding gasoline in general… https://www.cbsnews.com/news/gas-shortage-panic-colonial-pipeline-cyberattack/
-Opt in to Xeriscape Rebate Programs: A number of cities across the state offer programs that help rebate or mitigate the cost of replacing water guzzling lawns. Greeley, for example, will rebate $1 per square foot of bluegrass turf removed and replaced up to 2000 square feet! Obviously there are some stipulations and applications involved, but it is possible to receive money, use less water, and reduce time spent mowing every week. Check in with your City to see if they have similar options, and if not, reach out to City Council to see if they have plans or are interested in creating a similar program!
This is by no means a comprehensive list, so feel free to find methods that fit with your lifestyle. Even implementing just one of the above tips into your daily routine can make an impact on water usage, and leave you feeling happy with the effort you’ve made!
References:
1. https://water.usgs.gov/edu/activity-drip.html
2. https://www.greenamerica.org/save65gallons
3. https://www.watercalculator.org/footprint/the-hidden-water-in-everyday-products/
4. https://www.hgtv.com/outdoors/gardens/planting-and-maintenance/25-ways-to-conserve-water-in-your-garden-pictures
5. https://extension.colostate.edu/topic-areas/natural-resources/rainwater-collection-colorado-6-707/
*Tyler Eldridge is the Data and Asset Manager for the City of Greeley's Wastewater Treatment and Reclamation Facility, he also helps maintain the website and memberships for the RMWQAA.